In this article
- What Are Antibiotics?
- What Is Antibiotic Resistance?
- What Are Probiotics?
- Effect of Antibiotics on Your Microbiome
- Side Effects of Antibiotics
- The Microbiome Matters
- Taking Probiotics with Antibiotics Can Help
- 5 Tips for Taking Probiotics with Antibiotics
- Probiotics Instead of Antibiotics?
- Keep Your Gut Healthy
Note: This is a guest post from Jamie Morea
Even the healthiest among us will likely have to take an antibiotic at some point in our lives – whether it’s for strep throat, a tooth infection, or as a pre-surgery prophylactic.
The truth is that antibiotics are life-saving medicines, but they can do a number on our overall health.
From diarrhea and yeast infections to more serious inflammatory and immune conditions, antibiotics aren’t without their side effects.
The good news is that if you do need antibiotics for a bacterial infection, you can take steps to support your body during the process to minimize negative health consequences, including taking probiotics with antibiotics.
What Are Antibiotics?

Indeed, antibiotics are chemicals that either kill bacteria or prevent them from multiplying – stopping bacterial infections in their tracks or reducing them so our immune system can take over.
Sounds pretty lethal, right?
The good news is that antibiotics work by targeting certain features of bacterial cells, but they leave our human cells alone.
Some antibiotics prevent bacteria from building cell walls, and others interfere with their protein-building process.
Although most people credit the advent of antibiotics to Scottish biologist Alexander Fleming in 1928 with his discovery of penicillin, we now know that even ancient cultures used antibiotics to control bacterial infections.
Nearly 2,000 years ago, prehistoric Nubians brewed beer with Streptomyces, a tetracycline-producing soil bacteria (1).
What Is Antibiotic Resistance?
There’s no doubt that antibiotics have a crucial place in modern medicine, but their use does come with some significant downsides.
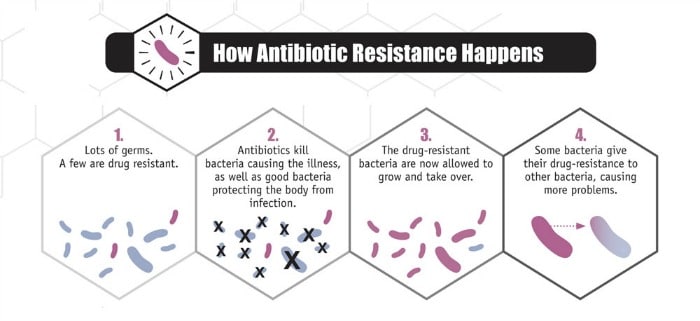
The overuse and misuse of antibiotics have led to antibiotic resistance, which is when bacteria become resistant to antibiotics.
This trait can be passed on from bacteria to bacteria – even among different species! – which leads to even more resistance.
Here’s how it works:
- Let’s say you have a population of harmful bacteria causing problems – some of these are naturally resistant to antibiotics.
- Antibiotics kill both the good and bad bacteria in your body, but the naturally antibiotic-resistant bacteria stand strong.
- Without all the antibiotic-susceptible bacteria taking up space, the resistant bacteria have room to multiply and they pass their resistance on to other bacteria.
- These “super bugs” no longer respond to certain antibiotics, leading to longer, more intense, and sometimes untreatable infections.
Source: Centers for Disease Control and Prevention
Every time we take antibiotics, more resistant bacteria have the opportunity to flourish – and some even become resistant to several different antibiotics, turning them into dangerous pathogens.
This is where taking probiotics with antibiotics can make a critical difference in your health.
What Are Probiotics?
From regulating your immune system and supporting your digestion and metabolism to crowding out pathogenic bacteria, balancing your blood sugar, and moderating your moods, the good bacteria in your gut positively impact your health in countless ways.
Probiotics work by crowding out or killing bad bacteria, producing enzymes and vitamins, communicating with your body’s cells, manufacturing brain chemicals like serotonin, sending signals to your brain, and regulating a large number of bodily processes.
We have more than 100 trillion bacteria in and on our body. All of these teeming colonies of microbes, both good and bad, make up a unique ecosystem called the microbiome.
Effect of Antibiotics on Your Microbiome
Even if antibiotics are prescribed responsibly – and by responsibly, I mean for serious bacterial infections, not viruses – they are associated with some significant negative health effects.
You see, in a balanced microbiome, probiotics comprise 85 percent of all the bacteria; that leaves only 15 percent of the bad guys. With beneficial bacteria solidly in the majority, your probiotics can work hard to keep you healthy and harmful bacteria are unable to gain a foothold.
But, what if antibiotics knock that probiotic percentage down to 50 percent, 40 percent, or even 20 percent?
Think of your gut as a parking lot full of spaces for bacteria to “park” and make a home. If the spots are full with mostly good microbes and a bad guy gets in, he has nowhere to park and must leave.
Antibiotics clear out the parking spaces, getting rid of most of the pathogens but wiping out the good guys, too. Now, what if a bad guy gets in? You guessed it – with plenty of open parking places, he (and all his friends) can settle in and take over.
Side Effects of Antibiotics
This sudden proliferation of bad bacteria and accompanying loss of the health-promoting good guys lead to a variety of antibiotic side effects, such as diarrhea, fungal and yeast infections, and inflammation – all of which can open the door to a wide variety of serious health issues.
That’s because by weakening your body’s probiotic makeup, antibiotic use also weakens your immune defenses.
A staggering 80 percent of your immune system resides in your gut where your probiotic bacteria work to regulate nearly every aspect of your immune function.
This also explains why it’s common for antibiotic use to lead to recurrent infections (and, of course, subsequent antibiotics), and why many people find themselves in a downward spiral of sickness, a vicious cycle that’s hard to break.
One side effect of repeated antibiotic administration is a Clostridium difficile infection. C. difficile is an opportunistic pathogen that thrives in the carbohydrate-rich environment of a gut cleared of its good microbes (2).
C. difficile (commonly called C-diff) is a potentially fatal microbe that secretes toxins that lead to diarrhea, fever, and colon inflammation.
Even though Fleming himself warned us of the dangers of antibiotic overuse, we’re only recently connecting these dots and beginning to make changes to both our paradigm and our habits – and the reason is twofold.
The Microbiome Matters
First, we’ve discovered the world under the microscope – our bacterial cells outnumber our human cells by a factor of 10:1.
We now understand the role our microbial health plays in our overall health and that a damaged microbiome can lead to a host of ailments such as poor immune function, mental disorders, obesity, and even chronic disease.
Second, we’re beginning to experience the realities of resistant bacteria firsthand.
The bad news is that just one course of antibiotics can negatively alter your gut microbiome and affect your odds of feeling your best.
In one recent study, researchers analyzed 66 individuals for 12 months after taking a course of antibiotics and found that the medication devastated the gut microbiome for up to a year.
Most apparent was the decline in short chain fatty acid-producing probiotics, which are important for controlling inflammation in the body. (3)
Taking Probiotics with Antibiotics Can Help
Although it may sound counterintuitive to take probiotic supplements while also taking probiotic-killing antibiotics, research shows that it’s beneficial to your gut health to fortify your system with the protective good guys.
In one recent review, patients taking probiotics during a course of antibiotics saw a whopping 60 percent reduction in the risk of contracting a C. difficile infection (4).
In another study, adults and children who took the probiotic Lactobacillus rhamnosus during antibiotic treatment had a 10 percent less risk of contracting antibiotic-associated diarrhea (5).
Even in people who do experience diarrhea when taking broad-spectrum antibiotics, probiotic supplementation reduces the duration of symptoms by an entire day (6).
Probiotics may also help prevent widespread antibiotic resistance by ensuring that people take their full course of prescribed antibiotics.
Stopping a course of antibiotics early – usually because of intolerable side effects – increases the chances that some of the bad bacteria may survive and become resistant. By reducing or eliminating side effects, probiotics can make it much easier to stay the course (7).
Not too shabby for a bunch of microscopic friendly flora!
5 Tips for Taking Probiotics with Antibiotics
We know that taking probiotics with antibiotics can prevent and alleviate side effects, repopulate the gut microbiome, and minimize antibiotic resistance, but how do we mix probiotics and antibiotics without having them cancel each other out?
First and foremost, make sure your doctor has confirmed a bacterial infection that warrants an antibiotic intervention before rushing to fill your prescription.
If not, request a lab test to make sure – you’d hate to take a harsh, gut-damaging antibiotic for a viral infection that will clear up on its own.
If you and your doctor have decided that antibiotics are a necessity, including probiotics in your daily wellness routine will maximize your chances of staying healthy.
Here are our five tips for correctly taking probiotics with antibiotics:
1. Find a Multi-Strain Probiotic Formula
Taking a daily probiotic supplement is a smart idea even when you aren’t fighting an infection, but it’s especially important during and after a course of antibiotics.
Look for a high-quality formula with a variety of human-resident strains (those from the Lactobacillus, Bifidobacterium and Streptococcus families) to repopulate your gut, including strains like L. rhamnoses proven to help during antibiotic treatment.
Also, choose a formula that guarantees the live bacteria will survive the acid-filled journey into your gut – many probiotic products in standard veggie capsules only have a 4 percent survival rate.
2. Give the Antibiotics Some Space
Wait at least two hours after taking antibiotics before taking probiotics.
As antibiotics work their way through your system, they’ll try to destroy anything in their path, including your good bacteria. Waiting two hours gives the antibiotics time to pass through your body so the good guys can safely settle in.
3. Don’t Stop!
Even after you’ve finished taking your course of antibiotics, you have some rebuilding to do – remember, it can take an entire year for your gut to recover from the nuking effects of antibiotics.
To rebuild and repopulate, continue taking a high-quality probiotic supplement as long as you are able, preferably indefinitely.
4. Incorporate Other Probiotic Sources
During and after antibiotic treatment, your best bet is to get as many different strains of probiotics into your system as possible to keep out the bad guys.
[Related: 17 Recipes Full of Probiotic-Rich Foods You Need to Start Making]
A probiotic supplement should be your number one priority, but you can also indulge in yummy food-based probiotic sources to give your system a boost. Fermented foods and drinks including ultimate superfoods like kimchi, sauerkraut, kefir, and kombucha all pack a big probiotic punch.
5. Focus on Prebiotics
The good guys in your gut need to eat in order to stand up to the bad bacteria bullies.
Luckily, their favorite food source – prebiotic fiber – is in several common foods that are easy to incorporate into a healthy, whole-foods diet.
Bananas, apples, onions, garlic, Jerusalem artichoke, asparagus, and dandelion greens to help your good microbes thrive.
And remember, the more you focus on whole, plant-based foods, the better. Studies show that this type of diet can have a relatively quick effect on your gut microorganisms (in as little as 24 hours).
Probiotics Instead of Antibiotics?
As the field of microbial research continues to expand, we expect the future of medicine will include targeted probiotic prescriptions in lieu of antibiotics, and that antibiotics will be reserved for specific or emergency scenarios.
In fact, probiotics are already proving to be more effective than antibiotics at treating and preventing certain diseases and infections, such as mastitis.
In one study, researchers analyzed 352 women suffering from mastitis, a painful breast infection often associated with breastfeeding. After 21 days, women who took probiotics saw more improvement and fewer recurrences than those taking antibiotics (8).
Keep Your Gut Healthy
In the meantime, the best thing you can do to ensure long-term optimal health is focus on tending to your microbial garden by protecting and nourishing your good flora.
And, don’t forget to look out for antibiotics in your food! Farmers often use antimicrobial medications to fatten up their livestock, so if you eat meat, fish, or dairy, make sure it’s antibiotic-free.
It’s hard to fathom where we’d be without the life-saving power of antibiotics.
But, as we move forward responsibly – using antibiotics only when absolutely necessary and making sure to support our wondrous gut microbiome along the way – we can do so with confidence that we’re giving our entire body the fortification it needs to live a healthy and vibrant life.